Breathlessness
Breathlessness is a common symptom in palliative care affecting between 40% and 80% of patients from a variety of underlying diagnoses. The symptom itself is often multifactorial with significant psychological interplay as breathlessness is one of the more frightening symptoms a person may experience.
The first step in managing breathlessness, as with any symptom, is to assess the causes and triggers. There will need to be baseline investigations such as a chest X ray, blood tests, oxygen saturation levels and probably more targeted investigations such as CT scans, echocardiograms, and blood gases. A careful history will describe triggers both physical and emotional.
Once reversible factors have been addressed a therapeutic trial of interventions can be implemented to assess what works for an individual patient.
Non-drug treatments
- Communication to explore, explain and reassure
- Fan therapy (either handheld or standing) is beneficial in regaining control of breathing patterns due to the cool air moving across the face
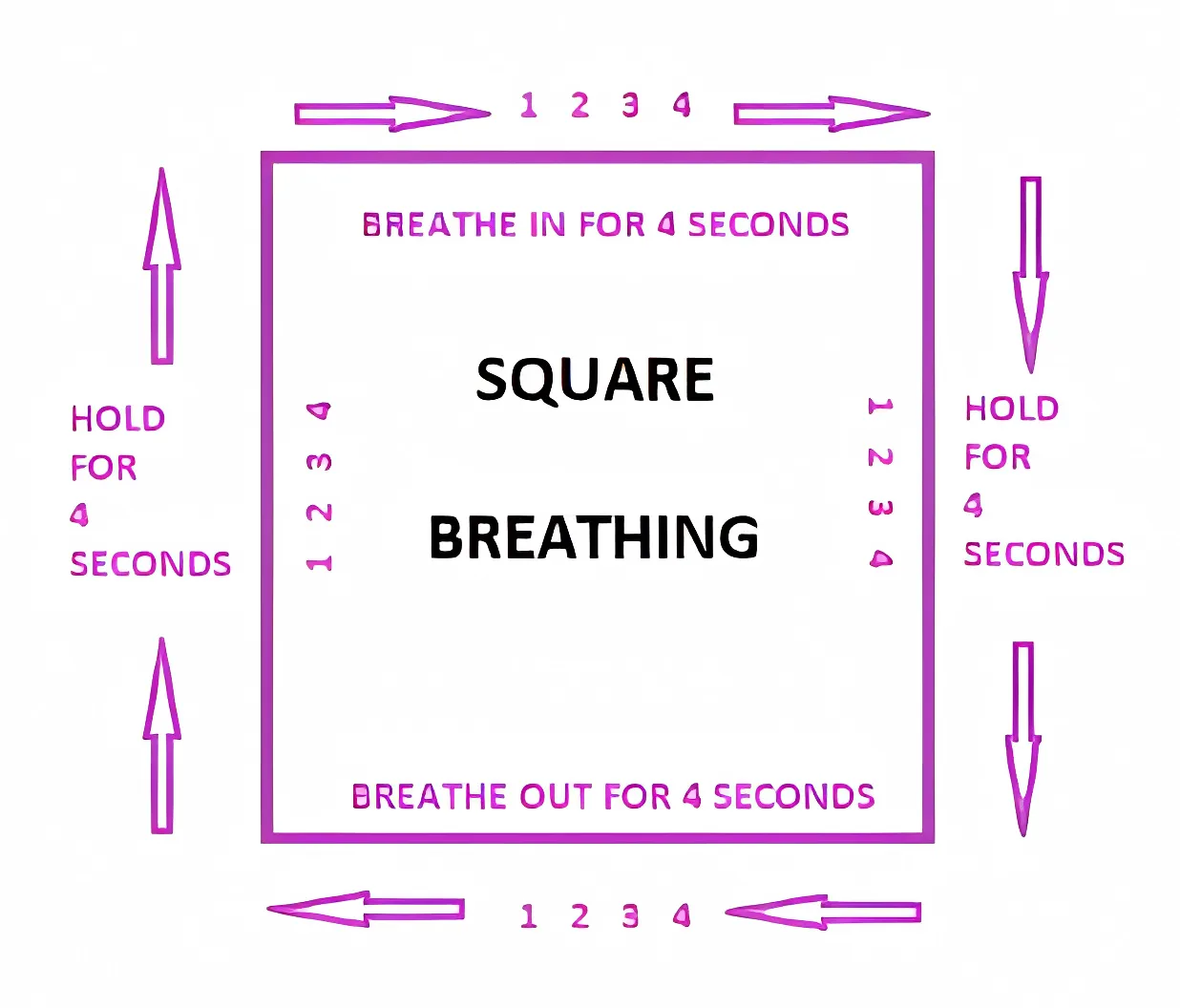
- Breathing exercises such as square breathing
- Visualisation
- Positioning
- Complementary therapies such as acupuncture, aromatherapy, or reflexology
- Pulmonary rehabilitation in either physiotherapist of nurse led service
Drug treatments
- Opioids can reduce the sensation of breathlessness; given in low doses (oramorph 1.25mg) four times a day. There is no indication that use in this way shortens life or compromises breathing
- Benzodiazepines (lorazepam 0.5mg) may be used alone or in combination with opioids especially when breathlessness is provoking anxiety and vice versa
- Oxygen has a variable effect of the symptom of breathlessness, and it is difficult to predict who will benefit so individual therapeutic trials are the only way to assess
- Care must be taken in patients with propensity for carbon dioxide retention
- Nasal cannulae are often preferred over masks as less confining, however nasal irritation may cause discomfort
- For some the burden of continuous oxygen attachment is too great without significant benefit
- Nebulised saline or other mucolytics are beneficial to those with difficult secretions
- Steroids for bronchoconstriction, superior vena cava obstruction, lymphangitis carcinomatosis