Pain
This is intended as a guide to management of pain in advanced and progressive disease, including both malignant and non-malignant conditions. It should not be used for managing chronic pain, which, although also multi-dimensional, requires long term management plans focusing more on psychological interventions and less on opioid use.
Pain is a complex symptom with influences from physical, psychological, social, and spiritual factors to create the experience of “total pain”. Some components of pain will not be amenable to analgesia and need to be assessed and treated alongside physical pain to achieve successful symptom control. The presence of non-physical aspects of pain often lowers the physical pain threshold.
In patients with cancer: one third will have a single pain, one third will have two pains and one third will have three or more pains. Experiencing multiple pains is equally common in non-malignant and co-morbid conditions and because of age, debility, and medical treatment.
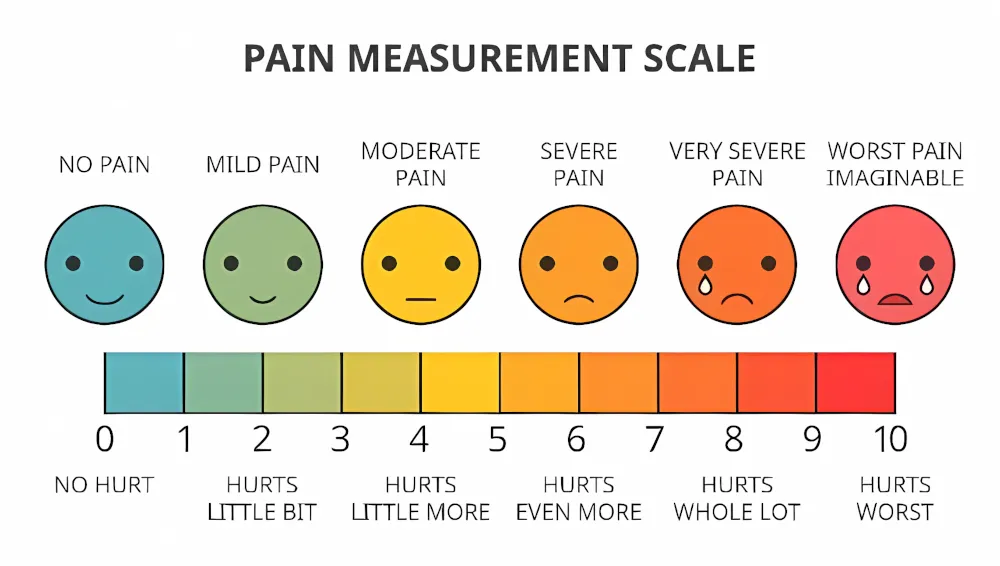
It is important to assess pains individually and form a diagnosis and treatment plan accordingly. Pain assessment tools such as a numerical rating scale or a visual analogue scale may help describe the severity of pain and can give a good indication of response to treatments. There are tools also available for assessment of pain in people with learning difficulties, dementia, and other communication issues.
Once a pain has been assessed and diagnosed, aim to treat using non-drug measures alongside the WHO Analgesic Ladder.
Non-drug treatments
- Relaxation techniques
- Distraction
- Heat pad
- Ice pack
- Psychological assessment and support
- Creative therapies
- TENS
- Acupuncture
Drug treatments
The WHO Analgesic Ladder was designed for treatment of cancer related pain; however, the principles can be applied to pain in any progressive, non-cancer conditions. These principles are:
- Use appropriate analgesic for the severity of pain
- Give analgesia regularly
- The preferred route of administration is oral for all “rungs”
- Progress up the ladder until pain control is achieved
- Remember to consider use of adjuvant analgesics (non-opioid drugs which can provide an analgesic effect especially alongside an opioid)
- Most opioids require co-prescription of laxatives
- Non-opioid analgesics are preferred in non-malignant conditions and those with a longer prognosis.
Adjuvant analgesics are medications whose primary indication is something other than pain relief but are known to have analgesic properties in some cases. Examples include steroids, antidepressants, bisphosphonates, and local anaesthetics. They can be used to enhance the effect of other analgesics, treat concurrent symptoms or to improve opioid responsiveness.
Opioids
- Recommended for moderate and severe pain, aiming use the lowest dose possible to achieve pain control while reducing the side effect burden
- Not always appropriate for chronic pain due to the risk of dependence
- The choice of strong opioid and appropriate dosing for severe pain depends on renal function, previous exposure, and physical condition
- Oral is the preferred route
- Not all pain will be opioid responsive, and some may respond better one opioid over another
- Starting doses can be roughly calculated by conversion to oral morphine dose from opioid currently in use to corresponding dose of chosen strong opioid
- Transdermal opioids can be useful in stable pain, especially if the oral route is difficult, however it is not suitable for acute or uncontrolled pain. Absorption will be affected by site of administration and cachexia. Reservoir patches must not be cut
- Always consider referral to specialist palliative care if effective pain control cannot be achieved even with rapid titration of doses, or where toxicity and side effects have limited doses
Opioid conversion calculator
Select drugs for dosage comparison.
- Morphine
- Oral
- mg
- 24h total
- 10
- 20
- 30
- 40
- 60
- 90
- 120
- 180
- Morphine
- Subcut
- mg
- 24h total
- 10
- 15
- 20
- 30
- 45
- 60
- 90
- Oxycodone
- Oral
- mg
- 24h total
- 10
- 20
- 20
- 30
- 45
- 60
- 90
- Oxycodone
- Subcut
- mg
- 24h total
- 5
- 10
- 10
- 15
- 25
- 30
- 45
- Diamorphine
- Subcut
- mg
- 24h total
- 5
- 10
- 15
- 20
- 30
- 40
- 60
- Alfentanil
- Subcut
- mg
- 24h total
- 0.5
- 1
- 1.5
- 2
- 3
- 4
- 6
- Fentanyl
- Patch
- Mcg/hr
- 72h
- 6-12
- 12
- 12-25
- 25-37
- 37-50
- 50-57
- Buprenorphine
- Patch
- Mcg/hr
- 7 days, unless indicated
- 5
- 20
- 15
- 20
- 35 (72h)
- 52.5 (72h)
- 52.5 (72h)
- Codine
- Oral
- mg
- 24h total
- 120
- 240
- Tramadol
- Oral
- mg
- 24h total
- 100
- 200
- 300
- 400
Neuropathic pain
There is often an element of pain due to dysfunction of nerves carrying pain signals, known as neuropathic pain. This may be due to compression of nerves (from spinal fractures/tumour), direct infiltration of nerves or inflammation of nerves (from infection, neuropathy). Neuropathic pain is often described as sharp, shooting or stabbing and there may be an associated area of altered sensation or function. Nerve plexus pain may present as a deep aching pain and usually does not have associated changes in sensation or function.
The difficulty of neuropathic pain is that it is often only partially relieved by opioid medications, if at all. Therefore, adjuvant analgesics are frequently required allowing lower effective opioid doses to be used.
Antiepileptics: Gabapentin
- Starting dose of 300 mg at night, increasing by 300 mg every 2-3 days to a maximum dose of 1200 mg three times a day.
- In the elderly or those with impaired renal function using starting and increment doses of 100 mg is preferred
- Side effects include sedation and delirium which may improve after the first few days, but can be intolerable for many patients
- The capsules are difficult to swallow but can be opened and sprinkled on food to assist in administration.
Antiepileptics: Pregabalin
- Starting dose 50-75 mg twice a day. This is increased every 3 days by 50 mg twice a day to a maximum total dose of 600 mg either 2 or 3 times a day
- Starting and increment doses should be reduced to 25 mg in the elderly or those with impaired renal function
- Side effects include sedation and delirium which may improve after the first few days, but can be intolerable for many patients
Other Antiepileptics such as carbamazepine or sodium valproate may be considered by specialist teams.
Antidepressants: Amitriptyline
- Start low with 10mg at night
- Can be increased to 25 mg after 3 days then weekly increments of 25 mg to a maximum dose of 150 mg at night
- Side effects include dry mouth, constipation, urinary retention and postural hypotension and increased risk of serotonin syndrome in combination with other serotonergic drugs
- Due to the extensive side effect profile not suitable in the elderly
- Alternatives in the same class (tricyclic antidepressants) include dosulepin, nortriptyline and lofepramine
Antidepressants: Duloxetine
- Start with 30mg at night but can be increased to a maximum of 60 mg twice a day
- Often better tolerated as fewer side effects but these can include dry mouth, constipation, and reduced appetite
Corticosteroids: Dexamethasone
- Useful for short term relief of pressure in spinal cord compression or nerve root compression
- Given in the morning to avoid insomnia and if needing a twice daily dose should be given morning and lunch time
- Given for 5-7 days to assess response and either stopped if no benefit or gradually weaned to lowest effective dose where it is helping
- Side effects include hyperglycaemia, gastric irritation and risk of ulceration, delirium, and fluid retention
- It is good practice to monitor BMs and co-prescribe a proton pump inhibitor (gastro protection) when on high dose corticosteroids
Benzodiazepines
- Examples include clonazepam and diazepam
- Lower doses needed in the frail elderly due to sedative side effects
- Dose increases may be limited by sleepiness and cognitive changes
- Diazepam can be of particular use when muscle spasm is contributing to pain
Others
- Capsaicin cream is manufactured from chilli peppers, applied to the site of neuropathic pain to hyperstimulate the nerves thus reducing their ability to send pain signals
- NSAID gels
- Lidocaine patches applied at the site of pain weakly anaesthetise the nerves. Must only be worn for 12 hours then removed for 12 hours to prevent local skin ischaemia due to the lidocaine effect
- Specialist options include methadone, ketamine, and interventional procedures